Technology
A New Dimension
Conventional 2D and 3D mammograms measure how many X-rays pass through the breast, yielding a single data point per pixel—density. Because cancers, gland tissue, and benign masses can share similar density, radiologists must look for subtle shapes or changes over time; this is why diagnostic precision is about 20%.
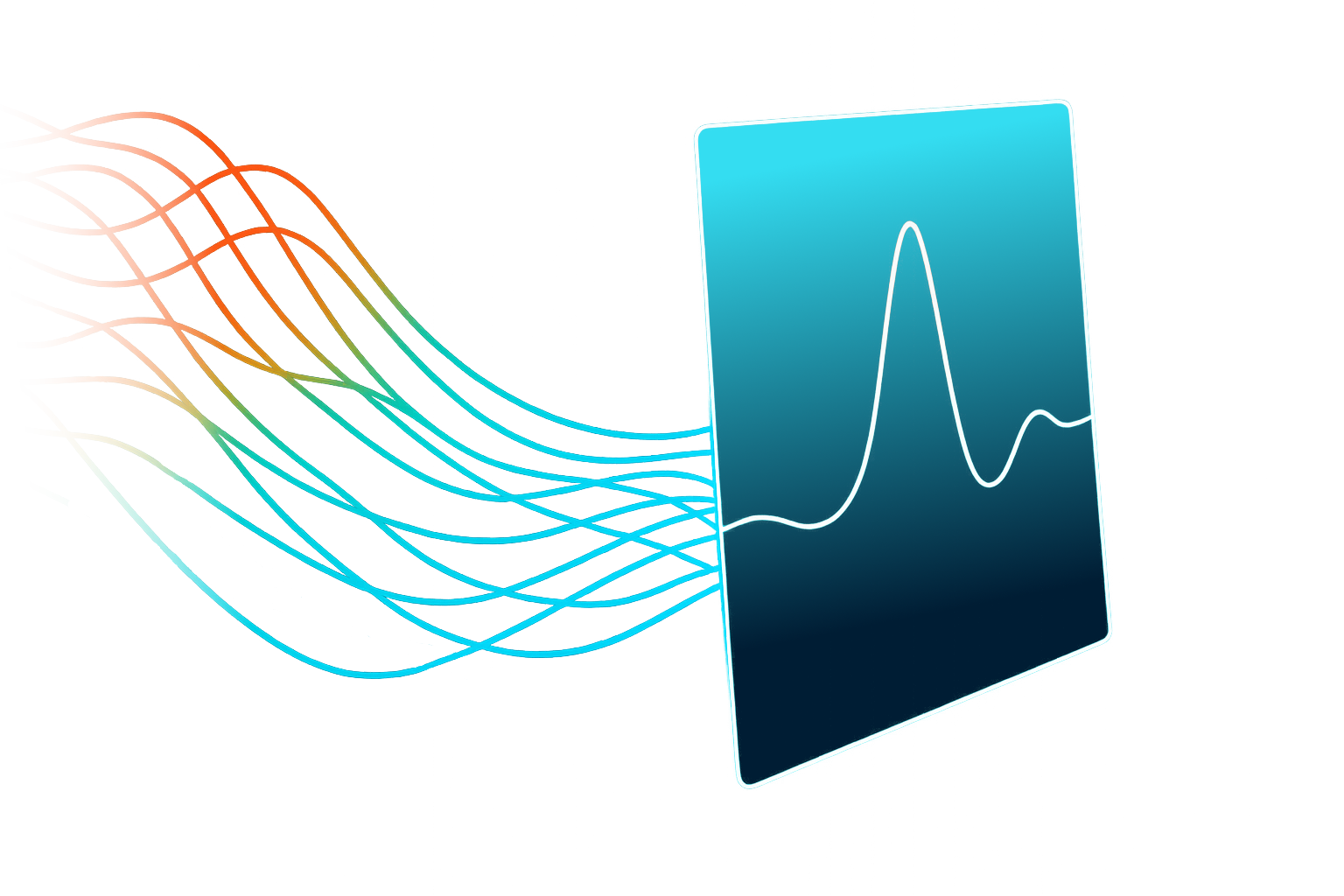
Calidar’s patented 4D Mammography combines 3D mammography with X-ray diffraction—the deflections X-rays undergo as they scatter from microscopic structures. X-ray diffraction measures many data points of X-ray intensity at different scatter angles, providing a wealth of information on tissue composition and structure.
Tissue Fingerprints
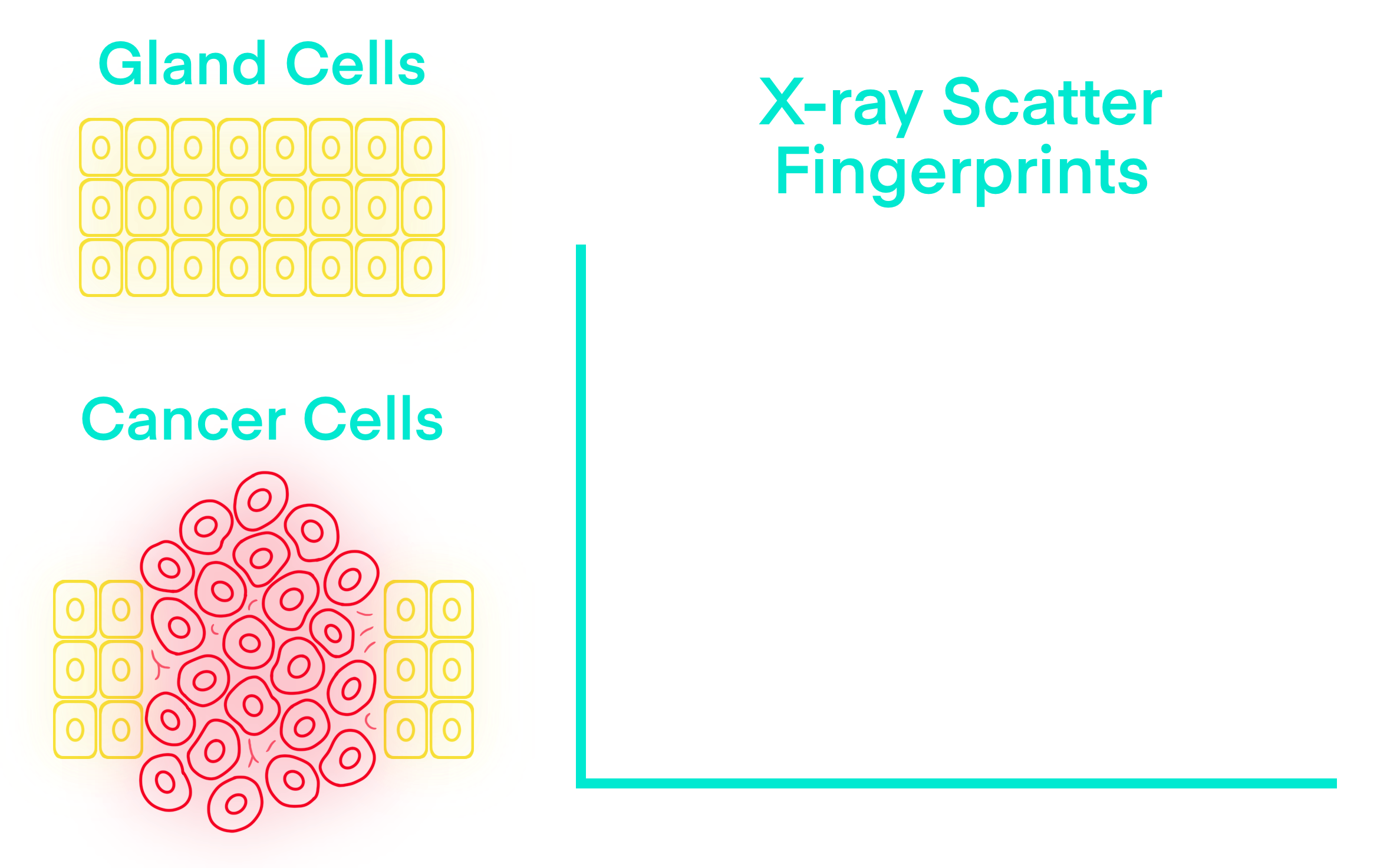
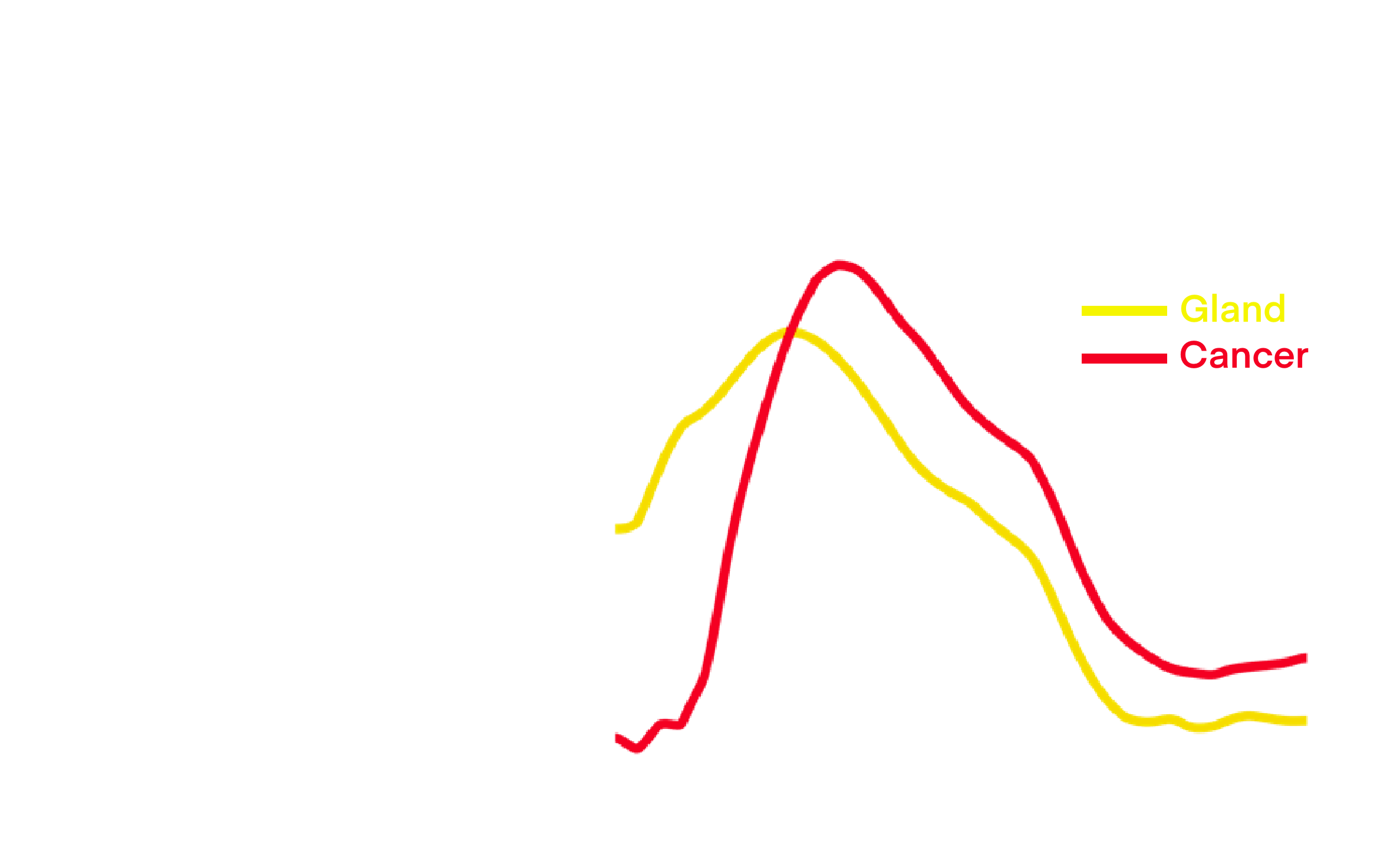
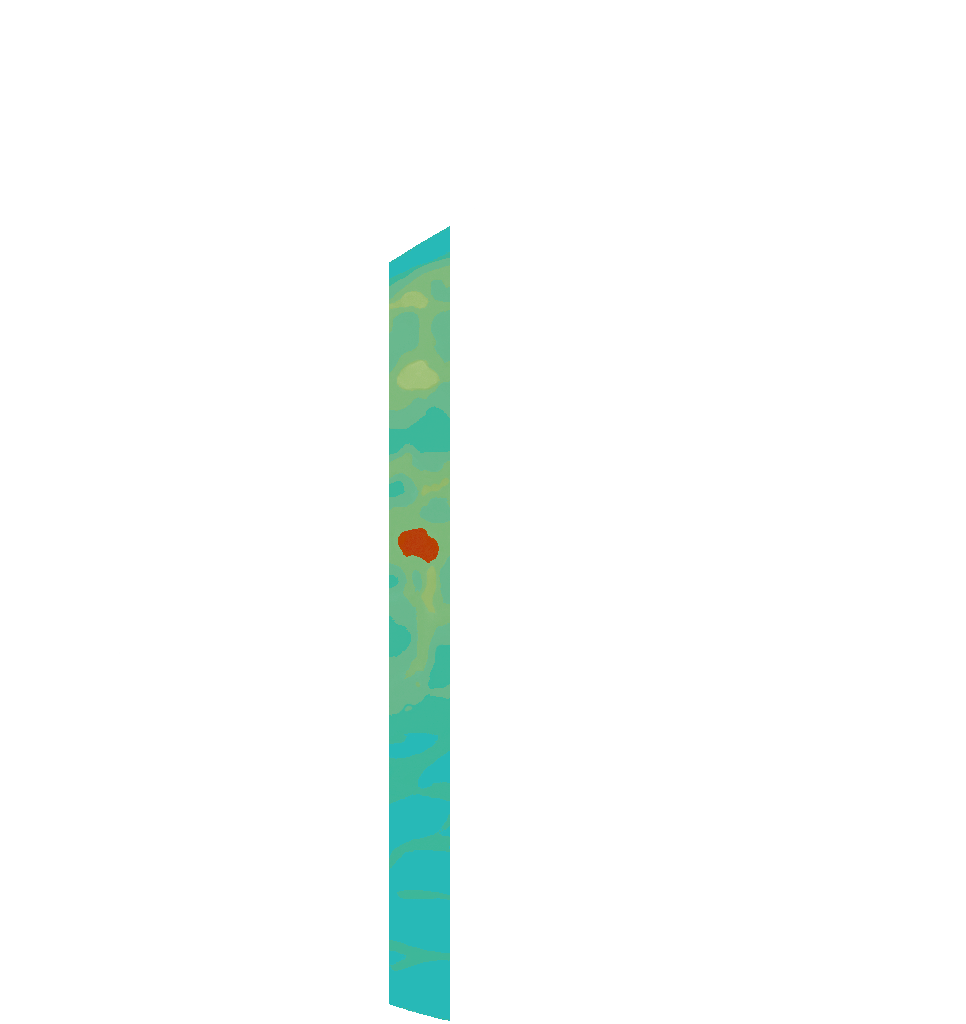
Different tissue types produce distinct X-ray diffraction spectra—characteristic profiles of scatter intensity versus angle, like a “fingerprint” of the tissue type.
Healthy gland tissue is well-organized, so its X-ray diffraction spectrum concentrates at lower angles. As cancer disrupts that order and cells proliferate, its X-ray diffraction spectrum shifts to higher angles (red curve), separating it from healthy gland (yellow).
From 3D to 4D
In density-based 2D/3D mammograms, cancer easily blends in with healthy gland tissue, while benign masses can appear cancerous— even though their cells look very different under the microscope, as pathology confirms after a biopsy.
4D Mammography adds another dimension to pixels in a 3D mammogram: their X-ray diffraction spectra, which reflect the structure and composition of the local cell environment. This 4th dimension—many data points per pixel—can be visualized in color; here, pixel color corresponds to the average diffraction angle, with red corresponding to higher angles, indicative of cancer.
The Value of 4D
Designed to fit current workflow, the goal of 4D Mammography is to provide physicians with new diagnostic insights noninvasively, without contrast injections, prior to biopsy. Prior results suggest X-ray diffraction could raise diagnostic precision from 20% to 80%, which could significantly reduce benign biopsies, "wait-and-see" surveillance, and delayed treatments that impact breast cancer survival rates.